| |
|
|
In Vitro Fertilisation (IVF)
 |
When the world's first IVF baby (called a 'test tube' baby at the time) was born in 1978 it brought hope to infertile couples across the world. Since then over one million babies have been born as a result of IVF treatment.
The Doctor's laboratory is one of the most experienced and best equipped in Thailand and has helped thousands of couples achieve their dream of having a baby.
IVF is involved in every Fertility treatment, or when other interventions you may have pursued in your home country have proved unsuccessful. |
IVF is used in a variety of situations including standard IVF treatment where a patient needs her eggs to be fertilized in a controlled environment; where PGD is needed to isolate genetic diseases; where the fallopian tubes are blocked; Egg Donation when the female partner has no viable eggs and her partner's sperm is mixed with the donor's eggs; when the male partner has low sperm volume and ICSI is used to inject a single sperm into an egg; where the woman is unable to carry a pregnancy (e.g. after hysterectomy) and her partner's sperm is mixed with either her or a donor's eggs and placed in a Surrogate uterus.
In Vitro Fertilization treatment usually follows these six stages:
First Stage - Pituitary Suppression
In a natural menstrual cycle, hormones from the pituitary gland, LH and FSH, stimulate the growth of an egg within a follicle in the ovary. Although several follicles start to grow each month, in a natural cycle only one will become mature enough to ovulate.
During an IVF cycle we want several eggs to mature simultaneously. At the same time we do not want an LH surge to trigger early release of these eggs. Doctor uses a medication known as a GnRH agonist to temporarily turn off your own LH and FSH secretion. This medication is usually started around day 21 of your menstrual cycle and continues throughout the stimulation phase. It is administered daily, usually by nasal spray or by injection.
Second Stage - Ovarian Stimulation
This is when daily injections of FSH begin. The injections continue for about 12-14 days and the amounts of FSH are higher than you would produce on your own. This is what stimulates the growth of several follicles, instead of just one. The response of your ovaries is monitored with frequent ultrasounds and blood tests. The dose and combination of medications is adjusted to your individual response and most women learn to give their own injections in order to reduce the number of clinic visits.
Up to 10% of women are unsuccessful in the ovarian stimulation phase. If your ovaries do not respond well enough, with too few follicles developing, the treatment cycle will be cancelled. The reasons for recommending cancellation will be discussed with you, along with options for further treatment, such as using an Egg Donor.
Third Stage - Egg Retrieval
Once your ultrasound indicates a reasonable size and number of follicles, the stimulation phase ends and the FSH injections and the GnRH agonist are stopped. That evening, an injection of hCG is given. This hormone causes the final maturation of the egg and loosening of the egg from the wall of the follicle. The egg retrieval occurs on the second morning after this final injection (34-36 hours later).
Retrieval of the egg is performed by an ultrasound guided needle puncture through the top of the vagina. The needle is passed into each follicle in the ovary and fluid is withdrawn into a test tube. The fluid from each follicle is examined under a microscope. Not every follicle contains an egg and not all of the eggs will be mature, but usually at least half of the large follicles will yield eggs.
The procedure itself will only take 10 to 15 minutes, but you will be asked to rest in the hospital’s recovery room for at least one hour afterwards. It is common to experience some cramping and discomfort after egg retrieval which can be alleviated with a light analgesic. Some mild vaginal spotting or bleeding may be present but will usually resolve within 24 hours.
The male role - Your male partner will be asked to produce his semen sample on the day of your procedure. It is understandable that some men may have experience 'performance anxiety'. If there is a real concern he can provide a sample a few days before the procedure to freeze until the day of fertilization.
Fourth Stage - Fertilization
 |
In some clinics natural fertilization is used where the sperm sample is washed and concentrated, then added to the eggs a few hours after retrieval. The dishes are placed in an incubator and eggs are examined the next day for signs of fertilization. Usually, about 70 to 80% of eggs are fertilized if the sperm sample is normal. The fertilized eggs are then kept in the incubator for an additional 48 hours. Not every follicle will contain an egg, not every egg will fertilize, and not every egg that fertilizes will become a good quality embryo |
Intra Cytoplamic Sperm Injection (ICSI) is a specialized form of fertilization used when your partner has a low volume of sperm. ICSI involves the injection of a single sperm directly into a mature egg. As up to 40% of cases of infertility are caused by male problems ICSI is now becoming a standard procedure in many clinics. ICSI is Doctor preferred choice for fertilization as it gives greater control over the fertilization process and generally results in higher rates of fertilization.
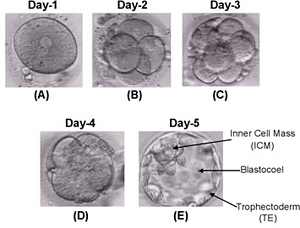
Fifth Stage - Embryo Transfer
Three days after egg retrieval, the fertilized eggs, now called embryos, are transferred to the uterus using a small catheter. The exact number transferred will depend on your age and your embryo quality. Generally Doctor recommends transferring two embryos as it is important to understand that the risk of multiple pregnancy increases with the number of good quality embryos transferred.
The embryos are placed in the transfer catheter which is passed through your cervix into your uterus where the embryos are gently released. The catheter is then slowly removed and checked under a microscope to ensure that the embryos have been transferred successfully.
You and your partner will be able to watch the procedure on the display screen in our transfer room. The transfer takes around fifteen minutes and you will experience only mild discomfort. Prior to transfer Doctor embryologist will have selected your two best embryos and the Doctor, or a member of his staff, will re-confirm the number with you on the day of the transfer. Some of your remaining embryos may be suitable for freezing, depending on their quality.
You will be prescribed Progesterone and Estrogen that you will need to take at the same time each day until you reach your 12th week. These will help keep your endometrium (the lining of your uterus) in optimal condition for implantation and maintenance of the pregnancy. The dosages and timings will be explained to you by the Doctor and his nursing staff.
You will need to rest for 2 days after the transfer but on the third day you will be able to travel home or continue your usual activities while you wait for your result.
Things to be aware of after embryo transfer that must be maintained until the 12th week
-
After embryo transfer, it is important that you keep to a healthy lifestyle.
-
Do not walk up steps in the first 3 days and be aware of not exerting yourself until your pregnancy test, 10 day post transfer.
-
If you have been taking folic acid tablets, you should continue to do so.
-
Do not smoke, take drugs, drink alcohol, coffee or strong tea
-
It is important that your core temperature does not increase so definitely No sunbathing, spas, saunas, jogging or aerobics.
-
No Sexual intercourse until the doctor advises otherwise.
-
Drink a lot of fluid and eat plenty of vegetables and proteins. Foods that are simple and easily digested are best.
-
Sometimes headaches can be the result of the hormone supplements so a mild analgesia such as Paracetamol may be taken if necessary.
-
Please contact our IVF nurse or the Doctor if you have any worries or concerns, or if you experience symptoms such as cramping or discomfort.
Stage Six - Luteal Phase and Pregnancy
The Luteal Phase is the 10-day period between the embryo transfer and the pregnancy test.
You may experience vaginal bleeding before you are due for your pregnancy test. Although this may be worrying, it does not always mean that the treatment was unsuccessful however, check with your doctor if you are concerned. Some bleeding can occur as a result of implantation of the embryo in the endometrium and is a normal part of the process. You should continue using the progesterone and estrogen until the blood test results are known 10 days after the transfer. Keep in mind that the progesterone you are taking may delay your period so not having your period does not necessarily mean that you are pregnant.
Waiting for results can feel like 10-months rather than 10-days and is often emotionally charged with expectation and anxiety. I understand this is a difficult time for couples and encourage you to contact me for support if you need reassurance.
Your Luteal phase is a time to spend sharing with your partner or friends doing activities that are pleasurable, relaxing but not taxing. Gentle walking, shopping, movies, and candlelit dinners together can help allay anxiety and help make it a positive time.
Contact IVF Bangkok 24 hours |
|